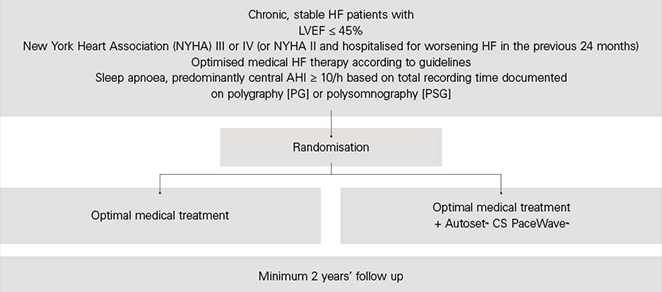
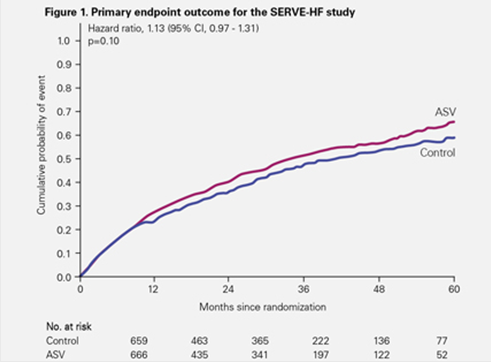
The SERVE-HF intention-to-treat analysis showed that ASV had no effect on the primary endpoint: composite of death from any cause, lifesaving cardiovascular intervention, or unplanned hospitalisation for heart failure (HF).1
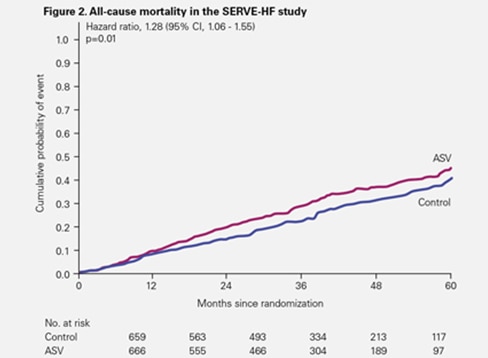
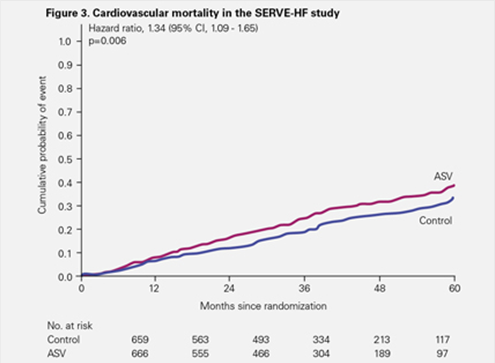
However, both all-cause and cardiovascular mortality occurred significantly more often in the ASV group.1
The cardiovascular death risk observed in SERVE-HF has been confirmed as a true clinical finding
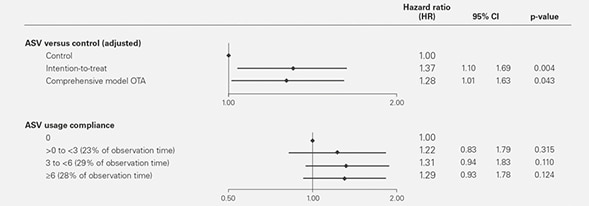
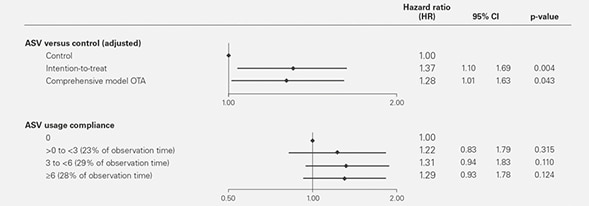
Following additional robust statistical analyses, it is now possible to discount any suspicions that potentially confounding factors – like low patient compliance with ASV or high cross-over between comparator arms – may have accounted for or substantially contributed to the observed mortality risk.2 The different on-treatment analysis confirmed that there was no impact of cross-over or compliance on the mortality risk in SERVE-HF.
The mortality risk was seen only in patients with systolic heart failure and predominant central sleep apnea
A robust statistical methodology called multivariate and multi-state modelling has been applied to SERVE-HF.3 The main findings are that:
- The risk is of sudden death, which is very likely to be arrhythmic
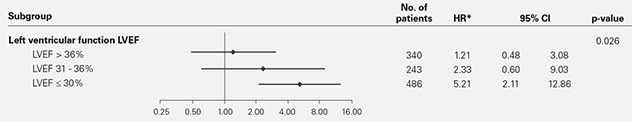
- There is a clear, statistically significant relationship between the mortality risk and the patient’s left ventricular ejection fraction (LVEF), i.e. the risk is greatest in those with the lowest ejection fraction.
- Associations between adaptive servo-ventilation therapy and cardiovascular death without prior hospitalisation for worsening heart failure or life-saving event
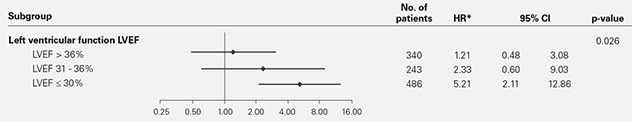
As a result, we can confirm that the observed mortality risk occurs in patients with LVEF ≤45% and that the harmful effects of ASV correlate with pre-existing LV systolic impairment.
* Adjusted for implantable cardioverter defibrillator (ICD), Cheyne-Stokes respiration (CSR) proportion at baseline and baseline left ventricular ejection fraction (LVEF).
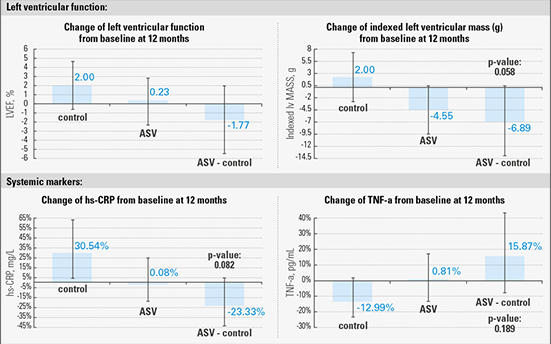
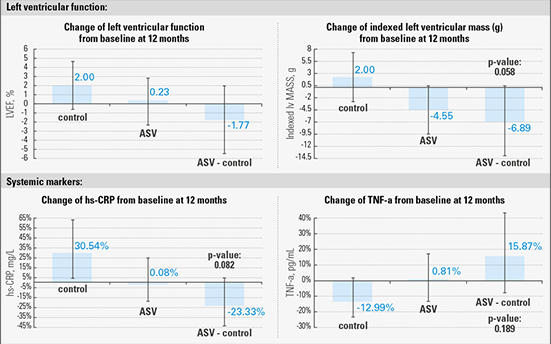
ASV may not worsen LV function3
The major SERVE-HF sub-study showed that ASV may have no effect on left ventricular function or remodelling and does not affect systemic markers associated with the heart failure syndrome, such as circulating neuro-hormones.
There was also no meaningful increase in hospitalisation due to worsening heart failure in the study.4 Therefore the possibility that the mortality risk might be attributable to deterioration in LV function appears remote.
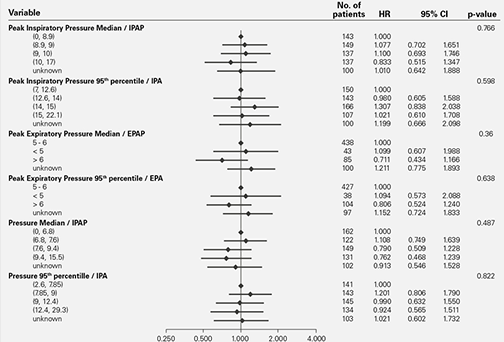
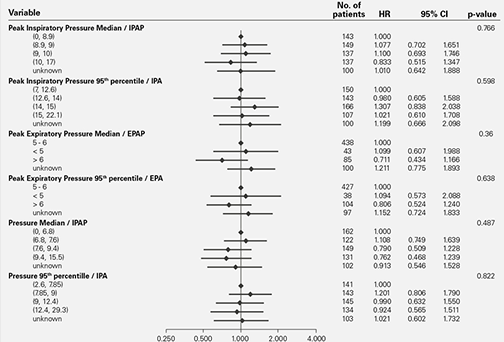
The mortality risk seen in SERVE-HF is unrelated to the magnitude of the PAP delivered5
The possibility that use of excessive inspiratory positive airway pressures might be to blame for the mortality risk also now seems remote. A new subgroup analysis has confirmed that the risk bears no relation to the magnitude of the inspiratory positive airway pressure delivered, which was individually adjusted for each patient in the trial.
Conclusion
We can therefore conclude that, in the presence of significant LV dysfunction and predominantly central sleep apnea, ASV may become a harmful intervention. People with enlarged and weakened left ventricles are a particularly vulnerable group, some of whom may also be at risk of sudden cardiac death from co-existing arrhythmias. In current clinical practice this has led to the increasing use of implantable defibrillators (ICDs).
ASV therapy is contraindicated in patients with chronic, symptomatic heart failure (NYHA 2-4) with reduced left ventricular ejection fraction (LVEF≤45%) and moderate to severe predominant central sleep apnea.
Patients with LVEF>45% continue to be eligible for ASV
Experts’ statements agree that patients with LVEF>45% remain eligible for ASV when there is a clinical rationale for using it.7,8,9,10